Translational Research in Digital Health and Gen AI
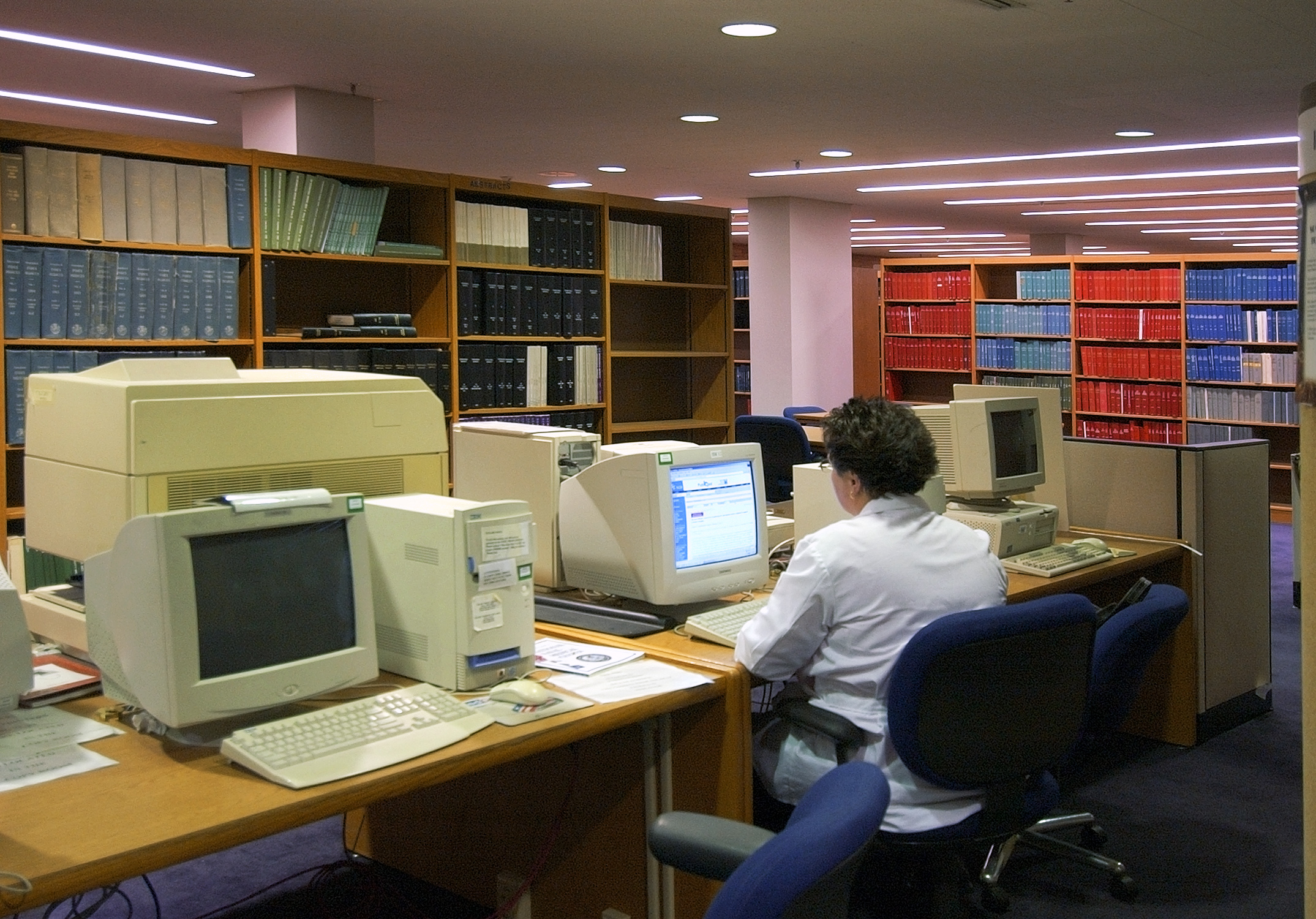
Translational research is the process of turning scientific discoveries into practical applications that can benefit society. It involves bridging the gap between different stages of research, from basic to applied, and between different stakeholders, such as researchers, clinicians, policy makers, and industry. Translational research aims to accelerate the transfer of knowledge and technology from the laboratory to the bedside, from the bench to the market, and from the ivory tower to the community.

Image credit: DoD Architecture Framework Working Group, Public domain, via Wikimedia Commons.
One of the key features of translational research is pragmatism, which means focusing on real-world problems and solutions, rather than abstract theories and models. Pragmatism also implies being flexible and adaptable to the changing needs and contexts of the target users and environments. Translational researchers are not satisfied with publishing papers in academic journals; they want to see their work make a difference in people’s lives and health outcomes.
Translational Research Methods & Techniques
To achieve this goal, translational researchers need to adopt a variety of methods and techniques that can help them design, develop, evaluate, and implement digital health solutions in an effective and efficient way. These methods and techniques include:
- User-centered design, which involves understanding the needs, preferences, and behaviors of the potential users and stakeholders of a digital health solution and involving them in the co-creation and evaluation of the solution.
- Rapid prototyping, which involves creating low-fidelity or high-fidelity prototypes of a digital health solution and testing them with the users and stakeholders in an iterative way, to obtain feedback and improve the solution.
- Pilot testing, which involves conducting a small-scale trial of a digital health solution in a real-world setting, to assess its feasibility, acceptability, usability, and preliminary effectiveness.
- Randomized controlled trials, which involve comparing the effects of a digital health solution with a control condition (such as usual care or another intervention) in a large and representative sample of participants, to determine its efficacy, safety, and cost-effectiveness.
- Implementation science, which involves studying the factors and strategies that influence the adoption, integration, and sustainability of a digital health solution in a real-world setting and developing and evaluating interventions to enhance these processes.
- Health economics, which involves analyzing the costs and benefits of a digital health solution from different perspectives, such as the users, the providers, the payers, and the society.
Translational researchers need to be aware of the latest advances and trends in digital health and related fields. One of the emerging paradigms in digital health is Gen AI. Gen AI refers to the development of artificial intelligence systems that can perform any intellectual task that a human can do, such as reasoning, learning, planning, decision making, and creativity. Gen AI has the potential to revolutionize digital health by enabling personalized, predictive, preventive, and participatory medicine, as well as enhancing the quality and efficiency of health care delivery and management.
Translational researchers play a crucial role in shaping the future of digital health and Gen AI. They act as translators, mediators, facilitators, and innovators between different disciplines, sectors, and domains. They also work as consultants for companies, organizations, and startups that want to develop, test, and implement digital health and Gen AI solutions. Translational researchers provide expert advice and guidance on the best practices and methods for designing, developing, evaluating, and implementing digital health and Gen AI solutions, as well as identifying and addressing the potential challenges and risks involved. Translational researchers also help to disseminate and communicate the results and impacts of digital health and Gen AI solutions to various audiences, such as academics, practitioners, policy makers, industry, and the public.
In summary, translational research is a vital and exciting field that aims to bring research papers into working artifacts, and to bridge the gap between digital health and Gen AI research and practice. Translational researchers adopt pragmatism as their guiding principle and use a variety of methods and techniques to design, develop, evaluate, and implement digital health and Gen AI solutions in real-world settings. Translational research is a practical endeavor that can make a positive difference in people’s lives and health outcomes.
Do you have a Gen AI research project that you need help with?